LIFE OF THE MIND
Stretching the Truth?
An examination of clinical laboratory tests for diseases involving gluten.
by Matthew Schoell

Does your favorite restaurant offer gluten-free options? Have you read articles extolling the health benefits of a gluten-free diet? American diet fads come and go. However, the market for gluten-free foods has increased dramatically in recent years, with estimates of billions of dollars. Gluten quickly gained a rather infamous reputation, formerly known for helping bakers by making bread dough stretchy and elastic. As medical laboratory professionals, we want to help patients and their providers make the best medical decisions possible. To that end, I became interested in how our clinical laboratories test for diseases involving gluten. Currently, two conditions are associated with gluten, celiac disease and non-celiac gluten sensitivity, but our laboratory testing for these diseases differs greatly.
For celiac disease, the picture is quite clear. Samuel Gee, a British pediatrician, first described celiac in the 19th century, noting the role diet played in treating the disease. Celiac is an autoimmune condition, where eating gluten triggers the immune system to inappropriately attack the intestines. The intestinal damage can lead to intense weight loss and even failure to thrive in children. Currently, the laboratory has two strong blood tests for the antibodies that develop in celiac disease, allowing for clear diagnoses. Unfortunately, celiac sufferers must remove gluten from their diet entirely to prevent dangerous immune responses.
For gluten sensitivity, the picture is much the opposite, as there are no laboratory tests for the condition. Early reports from gastroenterologists describe patients with nausea and fatigue after eating gluten, with symptoms reducing on a gluten-free diet. That simple picture became the subject of controversy in recent years, as the rates of gluten sensitivity appeared to explode in the United States population, driving the demand for the gluten-free food market. Bold claims appeared on both sides, that gluten-free diets provided health benefits to everyone or that the gluten-free diet was simply a fad.
The research into gluten sensitivity provides a confounding picture. Early reports in the 1980s and ’90s described small groups of patients, in much smaller frequency than people self reported in the 2000s. Much of what we do know about gluten sensitivity comes in the ways it differs from celiac disease. Gluten sensitivity is not an autoimmune condition and while associated with nausea and fatigue, it doesn’t cause the major weight loss or failure to thrive. While searching for the best literature on the topic, I turned to studies involving a controlled diet with either gluten or a placebo. There are very few such studies, and their results are inconclusive. In one example study, the researchers started with a pool of 140 individuals with gluten sensitivity, but quickly lost one-third of the participants when they showed no improvement on a gluten-free diet. Of the 98 remaining participants, only 28 had symptoms return on a diet containing gluten, and half of those 28 also had symptoms while taking the placebo.
So, what can these studies tell us about gluten sensitivity? There’s certainly reason to be skeptical, with so many participants’ symptoms not responding to removal or reintroduction of gluten. And all the studies using placebo diets showed that the placebos caused symptoms to return, raising the possibility that people’s perceptions can drive self-diagnosis with gluten sensitivity. And yet, there are some who continue to respond specifically to gluten-containing foods but are not celiac sufferers, who may well benefit from medical intervention (or possibly eliminating an alternative ingredient). As an educator in clinical laboratory sciences at Nazareth, I look forward to following the literature and continuing to educate students about gluten sensitivity and other developing challenges for the medical laboratory. Exploring these issues helps students understand the intersection between basic science research and the applied, clinical world and how their own scientific careers can contribute to the health of their communities.
Matthew Schoell, Ph.D., is an assistant professor of chemistry and director of the clinical laboratory sciences program.
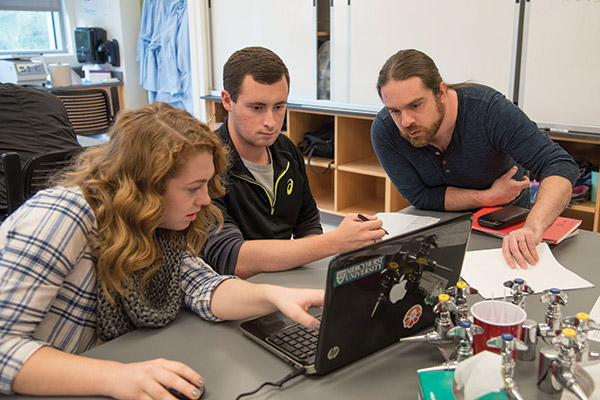
Matthew Schoell (right) assisting
chemistry students.